In today’s blog we continue to explore the different bruxism phenotypes.
Perhaps one of the biggest reasons for the confusion in the literature was the failure to differentiate sleep bruxism from bruxism occurring when awake.
Approximately one third of patients with SB also exhibit concomitant wake-time bruxism. The latter has an estimated prevalence of 12% in children and >20% in adults [1]. Psychosocial factors like stress, anxiety-hypervigilance and personality traits have significant influence on AB whereas there is less evidence to support their role in the pathogenesis of SB. The Polyvagal Theory (Porges, 1995)[2] which describes the development of the mammalian social engagement system and the involvement of the myelinated vagus, provide insights that suggest AB may be an effective adaptive strategy employed by certain individuals under stress to increase their ‘vagal brake’. The stoic socio-cultural environment (rewarding self-control, discouraging the open expression of emotions, keeping your mouth shut and your teeth together!) rather than genetics are thought to be responsible for significant racial differences in the higher prevalence of oral tori/bony exostoses in Asians [3, 4].
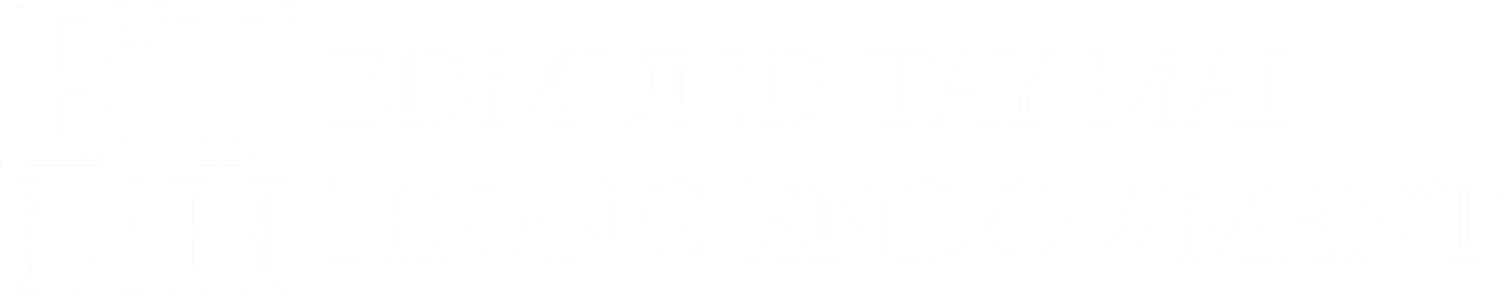
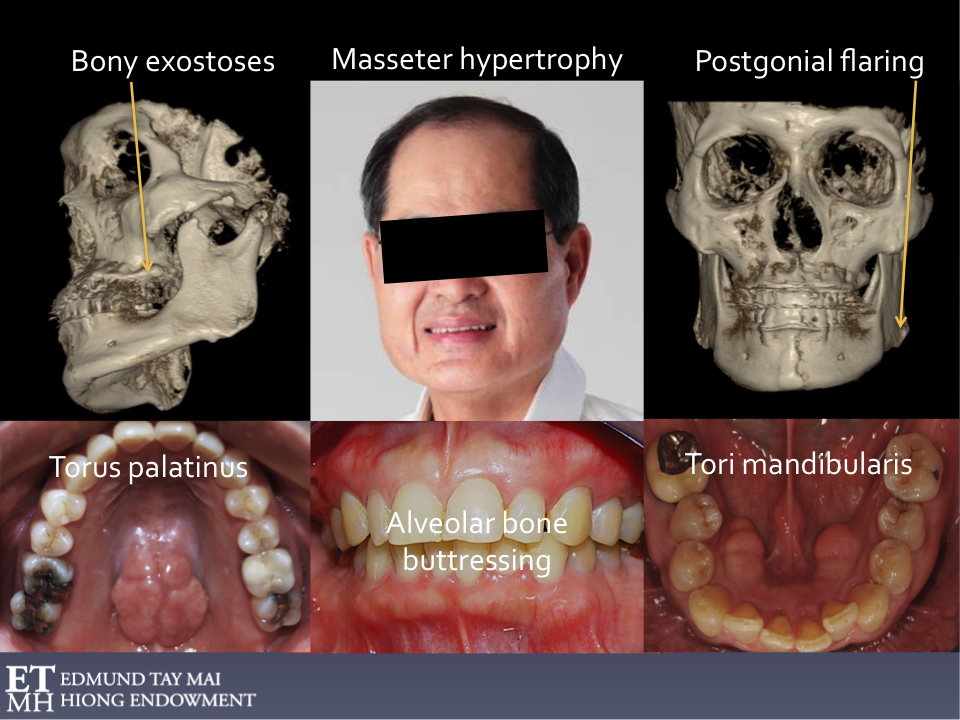
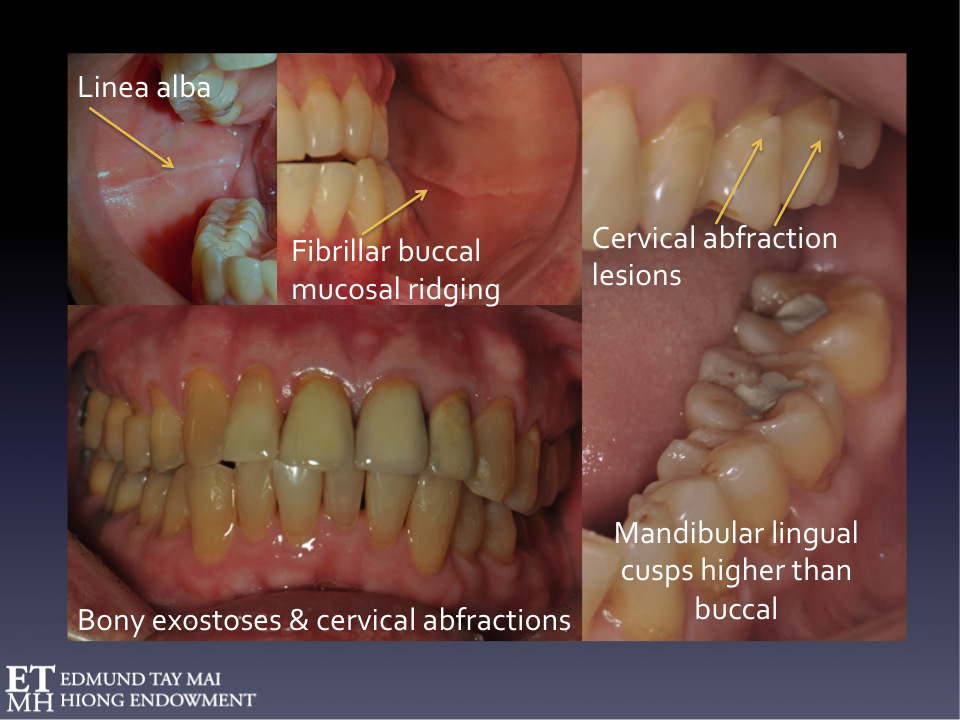
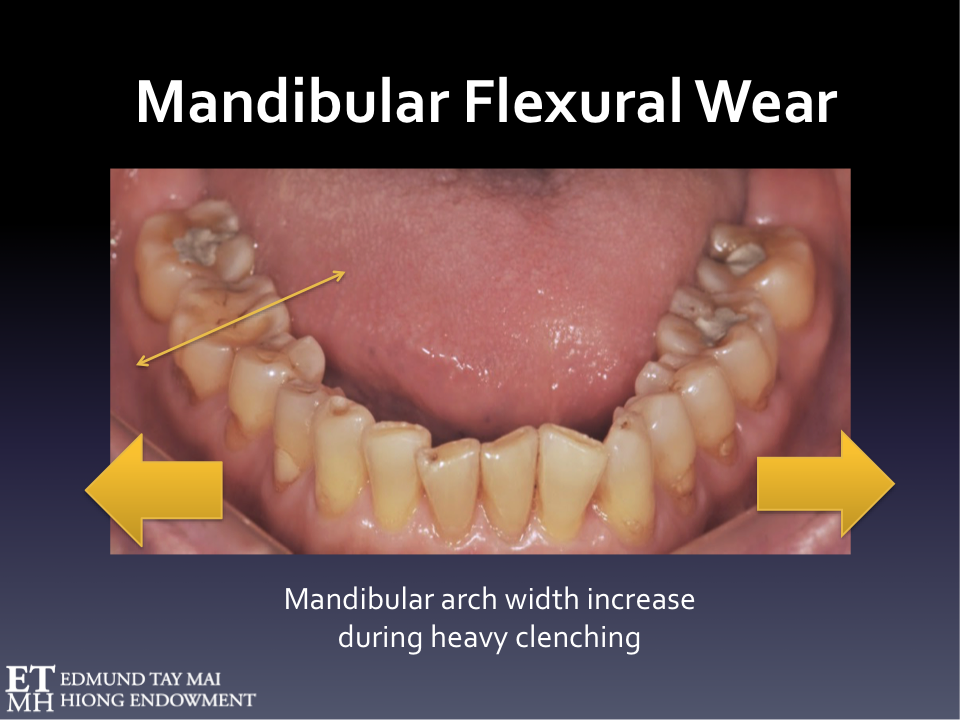
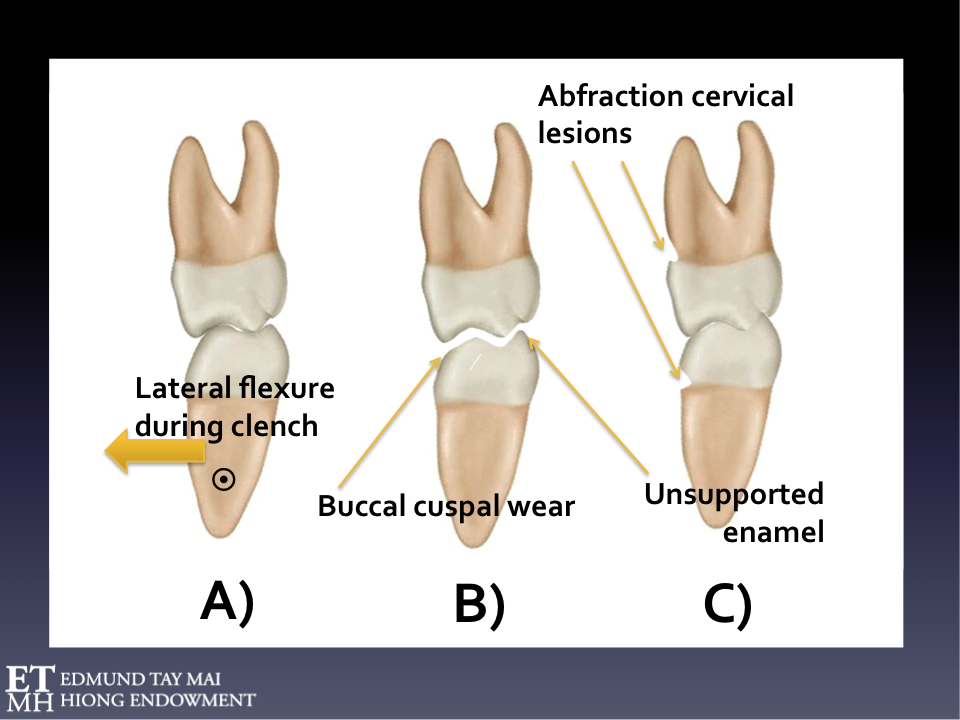
The prevalence of torus mandibularis and parafunctional jaw activity has been associated with temporomandibular disorders and migraine [5, 6]. Torus palatinus is another common clinical finding in subjects who engage(d) in eccentric tooth bracing (If you looked, you’ll always be able to find non-working side occlusal contacts!). As the mandibular transverse width (i.e. intermolar distance) increases with sustained centric clenching/bracing[7], the parafunctional lateral flexure of the mandible, besides contributing to the formation of lingual tori and other bony exostoses, also produces non-carious cervical abfraction lesions, dislodged fillings and pathognomonic tooth wear patterns where the lingual cusps are higher than the buccal. This mandibular flexural wear (Tay, 2012)[8] has often been incorrectly attributed to eccentric bruxism but these wear facets on the posterior teeth can also be observed even in patients with immediate canine disclusion. (Figs 7-10)
Fig. 7 Awake Bruxism
Fig. 8 Awake Bruxism
Fig. 9 Pathognomonic occlusal wear pattern related to lateral mandibular flexure associated with habitual (awake) parafunctional clenching
Fig. 10A Increase in mandibular width during clenching
Coactivation of bilateral hypertrophied temporalis and the pterygo-masseteric slings can cause intermolar distance increases during heavy clenching. The mandibular molar is carried buccally, repeatedly rubbing against opposing surfaces. Maximum lateral mandibular flexure occurring in the horizontal plane as reflected by a 0.5-0.6 mm increase in the intermolar distance has been estimated in chronic habitual clenchers.
Fig. 10B Pathognomonic mandibular flexural occlusal wear pattern
Involving the buccal facing inclines of the mandibular buccal cusps vs the lingual facing inclines of the maxillary buccal cusps & buccal facing inclines of the mandibular lingual cusps vs the lingual facing inclines of the maxillary palatal cusps.This hollowing out of the mandibular and maxillary occusal tables weakens the antagonists, leaves the unsupported enamel in the mandibular lingual cusps, and sharp edges all around. Prophylactic coronoplasty (e.g. creating more rounded cuspal morphology and reducing the tight grasping mortar-pestal intercuspation) will render the affected teeth less vulnerable to frictional wear/cracks/fractures and plastic restorations less prone to dislodgement and microleakage. The mandibular lingual cusps characteristically end up higher than the buccal in those engaging in severe habitual awake clenching.
Fig. 10C Compensatory eruption and formation of non-carious cervical abfraction lesion
As tooth surfaces wear, compensatory eruption will progressively ‘deepen’ intercuspation and the increased surface contact area during consequent function and parafunction leads to even greater frictional attrition and unfavorable stress concentration. The parafunctional forces repetitively generated during centric clenching create distinct stress shielding patterns that adversely affect enamel prism integrity at vulnerable cervical regions where prism orientation is different and the amelodentinal junction less scalloped. Notice the morphology of the mandibular cervical abfraction lesion is distinct from those found in the maxillary arch.
Buccal mucosal ridging is yet another interesting phenomenon associated with AB. Because the masseter muscle lies superficial to the buccinator muscle, the linea alba (or white line) commonly observed in chronic habitual clenchers is actually caused by pressure necrosis of the lining buccal mucosa trapped between the horizontal fibers of the buccinators. The masseters are activated wherever there is active posterior tooth contact, therefore a break in the mucosal ridging can be seen wherever there was an edentulous span. This clinical sign is testimony that the patient is continuing to (unconsciously) engage in this ‘perverse’ awake parafunctional habit. These buccal mucosal elevations will disappear, decrease in its severity, and/or morph when the posterior teeth are disengaged e.g. with use of a Nociceptive Trigeminal Inhibition(NTI) device, or if the clenching muscles are ‘chemically paralysed’ e.g. after administration of botulinum toxin type A.
Besides physically checking for these buccal mucosal giveaways, self-monitoring and habit reversal may be facilitated with the help of No Clenching (Live Ideas Creative Mobile Solutions Ltd), a free mobile phone application.
The Parotid-Masseter Hypertrophy Traumatic Occlusion Syndrome (Blatt, 1969)[9] is a relatively rare condition which occurs when the Stensen’s duct which passes through the buccinator muscles is occluded producing a mumps-like parotid gland swelling which lifts the earlobe. Knowledge of this phenomenon has helped me defuse, and on occasions, prevent medical-legal situations whereby anxious habitual clenchers were faced with multiple investigations/surgical interventions by medical colleagues unfamiliar with some of the more uncommon consequences of masseter hypertrophy.
Habitual repetitive submaximal contractions produces muscle hypertrophy in the elevator muscles and the rationale of our use of therapeutic Botox is that if the awake bruxer is not able to co-activate them for 3 months or so, intentional disuse atrophy and associated weakening would result. A habitual clencher can generate 5-6 times the voluntary bite force of a normal subject (measured via gnathodynamometer) whilst awake bite forces of 443 kg have been previously reported[10]. They are likened to trained Olympic athletes (where clenching is concerned) and although some experience end of day jawaches and headaches related to myofascial trigger points in these muscles, others do not report any symptoms whatsoever! In other words, it is the awake parafunctional activity that builds these strong muscles, but it is during SB episodes that the resultant movement vector and/or loads generated by them are unleashed. Thus, if the elevator muscles are somehow weakened and/or rendered unresponsive, the resultant stomatognathic tissue damage from both awake and sleep bruxism should be correspondingly less. Hypertrophied superficial masseter and temporalis muscles are commonly targeted when employing therapeutic Botox as they account for more than 75% of the bite force and seldom affect voluntary jaw movements other than gnashing. Associated phenomena (e.g. temporal headaches, jawaches, heterotopic odontalgia) related to active myofascial trigger points in these muscles, not uncommonly reported by awake bruxers, may also be simultaneously addressed. As was discussed in a previous blog, Botox reduces the amplitude but not the frequency of RMMA episodes.
Because of elevator muscle atrophy, some patients with AB would notice the improvement in frequency and severity of their daily ‘end of day’ jawaches and temporal headaches during active orthodontic treatment and might also report less morning symptomology attributed to concomitant SB (RMMA amplitude reduction) (Fig 11). Others may complain of the undesirable cosmetic consequences (e.g. looking gaunt) when temporalis and masseter muscles atrophy as their bracketed teeth become mobile and too uncomfortable to continue with their unconscious parafunctional behavior.
Fig. 11
Myogenous masticatory pain patients were found to have nearly 4 times more nonfunctional tooth contact during wake time than controls [11]. Long lasting muscle contractions may elicit muscle pain even if performed at low intensity. Despite strong clinical belief and dental school teaching that sleep bruxism is a causal factor in myofascial TMD, recent research [12] has provided new evidence that frequency of sleep bruxism was not increased for women with chronic myofascial TMD. Although self-reported rates of SB were significantly higher in case participants (55.3 %) than in control participants (15.2 %), PSG-based measures showed much lower and statistically similar rates of SB in the two groups. Thus, wake-time parafunction and central sensitization are now believed to be more relevant risk factors for persistent myofascial TMD than sleep bruxism [11, 12]. Therefore a good argument can be made for the supervised use of anterior midline point stop devices like the NTI or newer versions like the Flexi Orthotic System(FOS) in the management of awake bruxism.
The fact that the AASM clinical diagnostic criteria for Sleep Bruxism (ICSD-2, 2005) listed Hypertrophy of the masseter muscles on voluntary forceful clenching proved that until recently even the ‘authorities’ responsible for setting the guidelines were confused! Tonic RMMA episodes, even in patients with the most severe sleep bruxism, are never sustained for long enough periods to cause muscle to hypertrophy. Therefore, masseter hypertrophy and the formation of tori, bony exostoses, cervical abfractions etc can only be byproducts of Awake Bruxism when parafunctional posterior teeth bracing/clenching typically can exceed hours, whereas the average total functional tooth contact duration per day in the normal cohort is reportedly only 17.5 min [13]. The parafunctional jaw activities exhibited by many depressed patients and insomniacs who lay awake and restless in bed are often incorrectly attributed to sleep bruxism simply because it occured nocturnally. This may seem obvious but without PSG the distinction is sometimes difficult to make.
On the other hand, it can also be taken to mean that masseter hypertrophy might be one of the identifiable risk factors that transforms RMMA from being a physiologic adaptive behavior into its maladaptive form by increasing the intensity of the involuntary recurrent muscle contractions during sleep. Therefore, strategies to bring the strength of the symptomatic patient’s jaw elevator muscles into the normal range, and/or reducing the amplitude of RMMA, seem rationale.
Philosophically, when one takes into consideration the multiple systemic side-effects of anxiolytic and antidepressant medications that plague Western societies, masseter hypertrophy and a few cracked teeth might not sound like such a bad exchange!
Secondary Bruxism
We have always to be vigilant that we’re not actually dealing with a secondary bruxism i.e. comorbid sleep disorders, neurologic or psychiatric conditions, GERD, drugs/chemicals that may induce tooth grinding and/or clenching during wake or sleep. In an retrospective questionnaire study[14] of 900 patients from a neurological practice, 51% of responders reported the full triad of restless limb syndrome RLS), migraine headaches and sleep bruxism which led the author to suggest that SB to be a ‘restless jaw’ syndrome and RLS ‘a migraine in the limbs’! Dr. Dickoff provocatively advocated that all patients with sleep bruxism and RLS should be given a trial of dopaminergic agonists and insinuated that dentists have been negligently treating neurological disorders with structural therapy.
I’ve had on several occasions to deal with severe bruxism (both SB as well as AB) in children who were on methylphenidates e.g. Ritalin, Concerta for attention deficit hyperactivity disorder(ADHD) [15]. Despite the obvious damage to their dentition, in competitive Singapore, oftentimes it is their demanding parents who want them to continue with the drug till they finished school/university! Similarly I’ve had to consult with psychiatrists whose patients suffer serious phasic SB as a side-effect of serotonin specific reuptake inhibitors (SSRIs) like fluoxetine to either alter the dosage or change to another antidepressant.
A well-controlled PSG study of jaw muscle activity during sleep in patients with idopathic REM sleep behavior disorder (RBD) and Parkinson disease patients with RBD found an alarming 25% exhibited more rhythmic masticatory muscle activity during REM sleep[16]. The authors concluded that RBD should always be suspected and further neurologic assessment recommended whenever we encounter REM sleep bruxism.
Because the etiology of bruxism is not fully understood, there are those who advocate that the treatment of SB should be palliative. The following is one case to illustrate the error of such an approach.
In 1989 when I was still working in NUS, I had seen a teenager with severe REM SB with complaints of severe myalgia and TMJ arthralgia on waking. She frequently complained of vivid, action-filled dreams and involuntary limb movements during sleep. She did remarkably well on a stabilization splint but stopped appliance therapy after a relatively pain-free year on advice of her ill-informed dentist who believed that her pains were psychogenic in nature. She found me again in my private practice in 1995 when all her symptoms resurged and in addition she now had a huge anterior open bite(AOB). She was diagnosed with Idiopathic Condylar Resorption[17] - a relatively uncommon degenerative TMJ disorder seen mostly in adolescent females and young women. Currently, concomitant chemical and mechanotransduction processes are thought to be the major factors that can trigger the onset of progressive condylar resorption(PCR). Serum 17β-estradiol has an important osteoprotective effect in enhancing osteoprogerin expression and decreasing osteoclastic activity. The combination of low serum estradiol and overloading from recurrent nocturnal microtrauma of REM SB likely exceeded the adaptive capacity of the temporomandibular articular tissues in this case. Together with an orthodontist and a neurologist colleague specializing in movement disorders who put her on a maintenance doze of Clonazepam 1-1.5mg o.n., we successfully managed her AOB and proposed she wears a SomnoDent Mandibular Advancement Splint post-orthodontically to protect her compromised joints from further occlusal loading during REM SB episodes whilst also serving as an orthodontic retainer.
I insisted that she undergo a full night level I PSG study although the patient and her parents were reluctant and preferred I merely continued treating her symptomatically. When they finally agreed, she was slowly weaned off her nightly Clonazepam medication in preparation for the overnight study. This apparently unmasked a late onset epileptic seizure and she was subsequently referred for a MRI scan which discovered a dysembryoplastic neuroepithelial tumour (DNET) in her left frontal lobe bordering the interhemispheric fissure. This slow growing primary brain tumour was likely responsible for epileptiform activity in the frontal lobe manifesting as REM SB-like oromotor behavior since her teenage years. If not for my persistence, this obviously secondary bruxism may have never been confirmed. Can you imagine how recklessly inappropriate it would have been for us to continue managing a brain tumour with a piece of plastic!
Always, always, follow-up on patients who exhibit REM SB.
References
Manfredini, D., et al., Epidemiology of bruxism in adults: a systematic review of the literature. J Orofac Pain, 2013. 27(2): p. 99-110.
Porges, S.W., Orienting in a defensive world: mammalian modifications of our evolutionary heritage. A Polyvagal Theory. Psychophysiology, 1995. 32(4): p. 301-18.
Ohno, N., T. Sakai, and T. Mizutani, Prevalence of torus palatinus and torus mandibularis in five Asian populations. Aichi-Gakuin dental science, 1988. 1: p. 1.
Kerdpon, D. and S. Sirirungrojying, A clinical study of oral tori in southern Thailand, prevalence and the relation to parafunctional activity. European journal of oral sciences, 1999. 107(1): p. 9-13.
Sirirungrojying, S. and D. Kerdpon, Relationship between oral tori and temporomandibular disorders. International Dental Journal, 1999. 49(2): p. 101-104.
Clifford, T., P. Lamey, and L. Fartash, Mandibular tori, migraine and temporomandibular disorders. British dental journal, 1996. 180(10): p. 382.
Omar, R. and M.D. Wise, Mandibular flexure associated with muscle force applied in the retruded axis position. J Oral Rehabil, 1981. 8(3): p. 209-21.
Tay DKL, Dental Sleep Medicine: Its impact on prosthodontic practice and TMD management. 1-day workshop organised by the Australian Prosthodontic Society, Perth WA September 7, 2012.
Blatt, I.M., The parotid-masseter hypertrophy-traumatic occlusion syndrome. Laryngoscope, 1969. 79(4): p. 624-37.
Gibbs, C.H., et al., Limits of human bite strength. Journal of Prosthetic Dentistry, 1986. 56(2): p. 226-229.
Chen, C.-Y., et al., Nonfunctional tooth contact in healthy controls and patients with myogenous facial pain. Journal of orofacial pain, 2007. 21(3).
Raphael, K.G., et al., Sleep bruxism and myofascial temporomandibular disorders: a laboratory-based polysomnographic investigation. The Journal of the American Dental Association, 2012. 143(11): p. 1223-1231.
Graf, H. and H.A. Zander, Tooth contact patterns in mastication. Journal of Prosthetic Dentistry, 1963. 13(6): p. 1055-1066.
Dickoff, D.J. and S.M. Dontje, Restless limbs syndrome (RLS), migraine and bruxism: A common clinical triad. Annals of Neurology, 2013. 74: p. S47.
Winocur, E., et al., Drugs and bruxism: a critical review. Journal of orofacial pain, 2003. 17(2).
Abe S, Gagnon J-F, Montplaisir J Y, Postuma RB, Rompre P, Huynh NT, Kato T, Kawano F, Lavigne GJ. Sleep bruxism and oromandibular myoclonus in rapid eye movement sleep behavior disorder: a preliminary report. Sleep Med, 2013. 10: p.1024-30.
Gunson, M.J., et al., Oral contraceptive pill use and abnormal menstrual cycles in women with severe condylar resorption: a case for low serum 17β-estradiol as a major factor in progressive condylar resorption. American Journal of Orthodontics and Dentofacial Orthopedics, 2009. 136(6): p. 772-779.
The views and opinions expressed in this article are those of the author's alone.